Erik Sutherland, East Renfrewshire CHCP
In East Renfrewshire CHCP we have been reporting on Talking Points Personal Outcomes since 2009/10. The outcomes are included both in shared assessment and review documentation in our information system. In the assessment tool, there is space for an outcomes dialogue, which involves practitioners bringing together all the relevant information, including the person's views and outcomes, and drawing conclusions about what needs to happen. In the review, progress in realising outcomes is recorded as 'met', 'partially met' or 'unmet.' Quantitative reports are drawn from the core information system and reported to various strategic and operational groups in the CHCP.
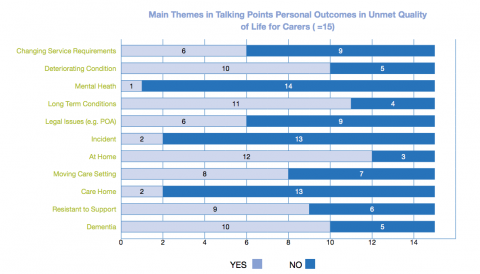
Early in 2012, through quantitative performance reporting, a deterioration in carers' personal outcomes was noted. We wanted to investigate the cause of this and a small-scale audit of unmet personal outcomes was agreed. This audit focused on the 15 carers involved in that quarter where outcomes were recorded as unmet (as compared to 91 met and 38 partially met). Two of us worked together to identify themes within the outcomes dialogue for carers where quality of life outcomes were unmet. We undertook a paired reading exercise and both agreed a number of main themes were arising. A matrix of these themes was then produced to form the basis of analysis (see image below).
In cases where carers' quality of life outcomes were unmet, it was found that the cared for person tended to live predominantly at home, with long-term conditions (commonly including dementia) which were often deteriorating. In addition, the audit found that 'resistance to support' was common and transition in care settings figured significantly - though not always from home to care home. Several qualitative comments served to illustrate these themes further. In one instance it was noted that 'personal care is a particular trigger'. In another, it was recorded that the cared-for person was 'reluctant to accept care…does not have insight into difficulties with self-care';. In another case, dementia was recorded as having 'reduced cognitive abilities to self-care' with 'care needs creating a high level of stress' for carers.
Within the qualitative data there was evidence of constructive dialogue between practitioners and carers and the people they cared for. It was evident in these dialogues that there was a focus on reviewing supports, enhancing insight, linking to community assets and promoting resilience in caring relationships to enable carers to be 'less anxious and isolated…[to]…reduce the pressure on the family and thus sustain [the cared for person] for longer at home'. The dialogues include consideration of different forms of short-break, telecare and alternative day opportunities being explored alongside transitions to care home.
We are already starting to use the information on outcomes to influence decision making within the CHCP. The information about carers' quality of life outcomes has provided an important feedback loop to commissioning processes and the development of more personalised short-breaks. Since the audit, performance on carers' quality of life personal outcomes has started to improve again.